Table of Contents
What is MDS
MDS is a simple, robust way to describe metadata, or information about data. In the MDS model all metadata are defined as semantic triples in the form subject-predicate-object. The three parts of the triple are all strings and may contain any character, including spaces. The subject and predicate together define a unique key for the triple.
Your MDS treatment depends on:
- Your age
- Your overall health and any other medical conditions.
- The type of MDS you have.
- The stage (extent) of the disease.
- Whether your blood cell counts are low.
- Whether you have symptoms.
- Whether your disease has progressed to acute myeloid leukemia or to another type of cancer.
- Your doctor will consider these factors when creating a treatment plan for you.
Treatments for MDS can include:
Watchful waiting. For people with low-risk MDS, doctors may recommend simply having regular checkups and blood tests to monitor the disease and ensure that it’s not progressing. This approach is especially common in elderly people who aren’t otherwise in good health and are likely to die soon from other causes.
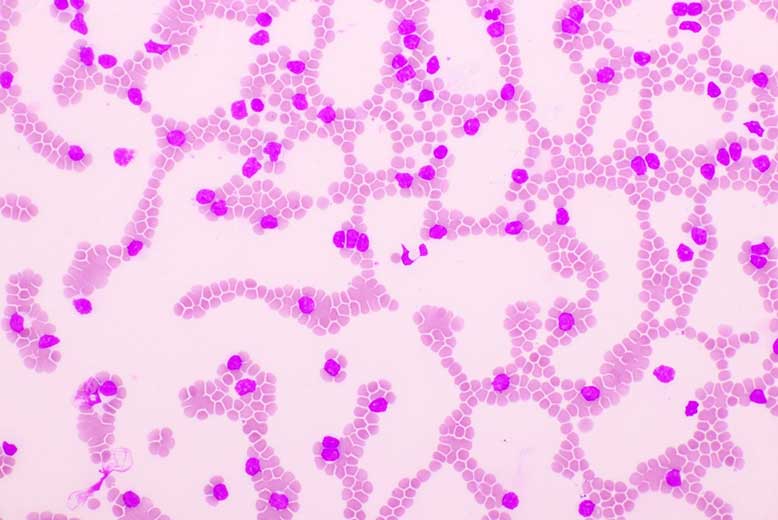
Certain blood transfusions. Doctors may suggest transfusions of blood components, such as red blood cells, platelets or plasma to help improve anemia or bleeding problems.
Growth factors. These drugs stimulate bone marrow to make more blood cells. Two common growth factors are granulocyte colony stimulating factor (G-CSF) and granulocyte-macrophage colony stimulating factor (GM-CSF).
Antibiotics, antivirals and immune therapy. These treatments might help boost your immune system to fight infection that results from low levels of white blood cells.
Chemotherapy. Medicines used in chemotherapy work by killing rapidly growing cancer cells. The drugs are usually injected into a vein (intravenously). In addition to destroying cancer cells, chemotherapy also kills healthy cells that divide quickly, such as those found in the bone marrow, GI tract and hair follicles.
MDS clinical trials
Disease-modifying therapy
Disease-modifying therapy is defined as treatment that can improve the bone marrow function, stop disease progression, or prolong survival. In the past, disease-modifying therapy for MDS was a simple concept, because only a small number of treatment options were available. Now there are many possible therapies, and their effects on survival and quality of life can be hard to predict.
Chemotherapy
These drugs work by killing rapidly dividing cells. They are not very effective at treating low-risk MDS because these cells do not divide rapidly. However, they may be used to treat high-risk MDS if it transforms into AML.
Induction therapy
The goal of induction therapy for MDS is to achieve remission and improve the blood cell counts. Remission is characterized by the absence of blast cells in the bone marrow. In addition, patients should have an increase in hemoglobin and platelet counts, and a decrease in transfusion requirements.
Patients with lower-risk MDS are considered for treatment with azacitidine or decitabine. These drugs have been shown to improve blood cell counts, transfusion requirements and quality of life in patients with lower-risk MDS.
Consolidation or intensification therapy
Consolidation or intensification therapy is a term used to describe treatment given to patients who do not respond adequately to initial treatment of low or intermediate risk MDS. The aim of consolidation therapy is to increase the number of normal blood cells present in the bone marrow and blood. This may be done by using blood growth factors to stimulate production of new blood cells, using more aggressive chemotherapy, using immunotherapy (treatment with drugs that boost the immune system), or by using stem cell transplantation.
Blood and marrow transplantation
Allogeneic hematopoietic stem cell transplantation is a treatment that replaces bone marrow that does not function properly with healthy bone marrow from a donor. The procedure, also known as blood or marrow transplantation, offers the possibility of a cure for MDS. However, it has an increased risk of complications and side effects compared to standard MDS treatments.
The patient’s blood cells may come from his or her own body (autologous transplant) or from a donor (allogeneic transplant). Allogeneic transplantation is used more commonly in MDS than autologous transplantation.
The goals of allogeneic transplantation are to:
- Destroy the abnormal cells with high doses of chemotherapy and/or radiation therapy
- Give healthy blood-forming cells to replace the abnormal cells destroyed by treatment
- Treat the patient with lower doses of chemotherapy so they can get back to feeling well quicker after their transplants
Allogeneic BMT
Allogeneic BMT (allo-BMT) consists of infusion of hematopoietic stem cells from an HLA-matched sibling donor, an unrelated donor, or a haploidentical donor (i.e., one who is half matched). Allogeneic BMT can be performed after high-dose chemotherapy/TBI as a myeloablative regimen or after nonmyeloablative conditioning, which includes low-dose TBI and immunosuppressive drugs but no cytotoxic chemotherapy. The main advantages of allo-BMT compared with autologous BMT are the potential for a graft-versus-leukemia effect and the lack of relapse. However, allo-BMT is associated with higher treatment mortality (see “Risks and complications”).
Autologous BMT
A bone marrow transplant (BMT) is a procedure to replace diseased or damaged bone marrow with healthy bone marrow stem cells. Bone marrow is the soft, spongy tissue in the center of your bones. It produces blood cells.
There are two types of BMTs: autologous and allogeneic. In an autologous BMT, you receive your own stem cells. The stem cells are collected from your blood or bone marrow before you get high-dose chemotherapy and radiation treatment. They’re stored until you’re ready for them after treatment. In an allogeneic BMT, you receive stem cells from a donor (allogeneic means “from another person”).
An autologous BMT may be an option for people with myelodysplastic syndrome (MDS) who have very low-risk disease that has not responded to other treatments and who are in good health. A BMT can damage the lungs, liver and kidneys, so it’s more risky for someone who has other serious medical problems.